
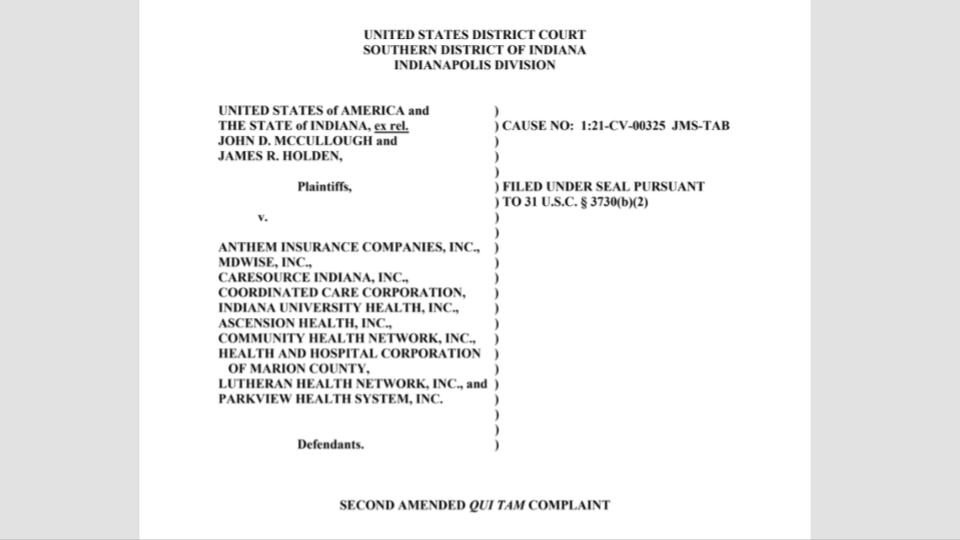
According to a report in the Indianapolis Star, a whistleblower lawsuit accuses several insurance companies and hospitals of defrauding Indiana’s Medicaid program of up to $700 million, potentially deepening the state’s nearly $1 billion Medicaid shortfall.
Filed by former state employees James McCullough and James Holden, the suit claims improper billing, duplicate claims, and payments for services provided after patients had died.
The lawsuit argues that state officials began limiting fraud recovery efforts in 2017 under political pressure from healthcare lobbyists, despite warnings from IBM Watson, the state’s fraud detection contractor. The reports, covering 2015 to 2020, identified hundreds of millions of dollars in suspected fraud, which the lawsuit alleges could have alleviated the financial crisis if recovered.
The alleged misconduct occurred as Medicaid faced rising costs, especially for home-based care programs, which state officials have blamed for the budget shortfall. However, McCullough and Holden argue that fraudulent activities, enabled by political connections, contributed significantly to the financial gap.
Insurance companies and hospitals involved in the lawsuit have largely denied the claims, while state legislators, including Rep. Greg Porter, voiced frustration over the unaddressed overpayments. The case, filed under state and federal false claims acts, seeks to recover lost funds for Indiana’s Medicaid system.




Leave a comment